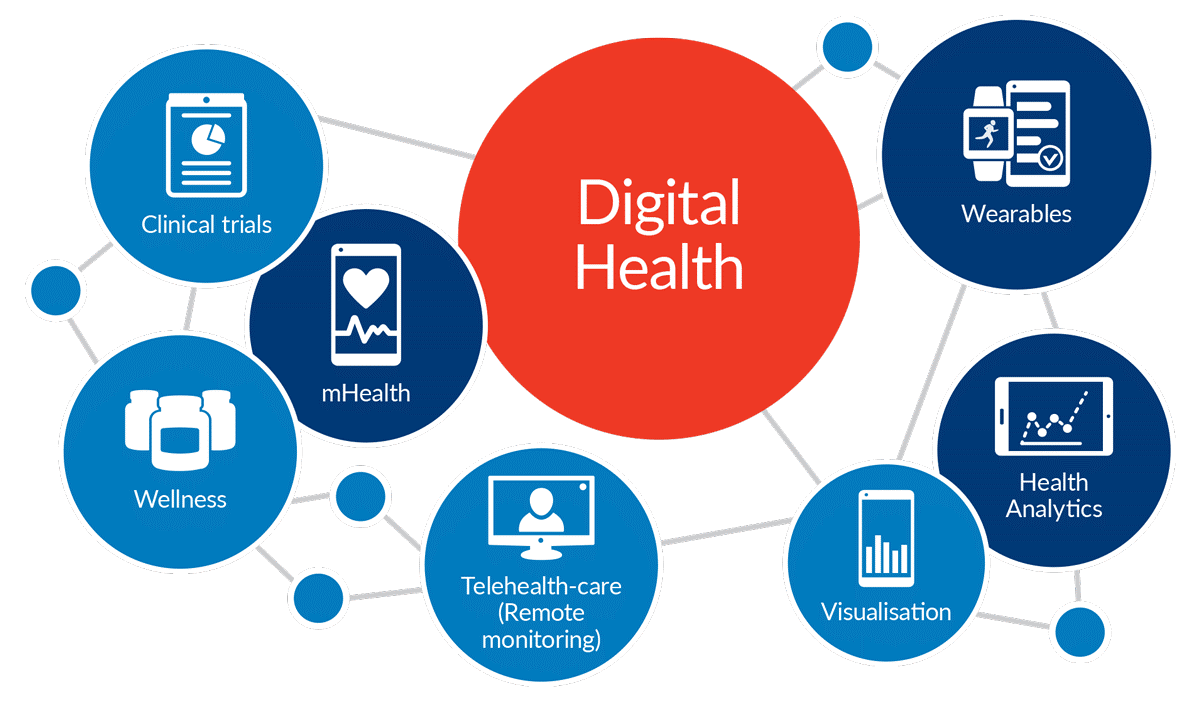
The convergence of science and technology in our dynamic digital era has resulted in the development of innovative digital health devices that allow easy and accurate characterization in health and disease. Technological advancements and the miniaturization of diagnostic instruments to modern smartphone-connected and mobile health (mHealth) devices such as the iECG, handheld ultrasound, and lab-on-a-chip technologies have led to increasing enthusiasm for patient care with promises to decrease healthcare costs and to improve outcomes. This ‘hype’ for mHealth has recently intersected with the ‘real world’ and is providing important insights into how patients and practitioners are utilizing digital health technologies. It is also raising important questions regarding the evidence supporting widespread device use. In this state-of-the-art review, we assess the current literature of mHealth and aim to provide a framework for the advances in mHealth by understanding the various device, patient, and clinical factors as they relate to digital health from device designs and patient engagement, to clinical workflow and device regulation. Within these early years of the 21st century, we have witnessed remarkable technological progress with the developments of powerful and portable computing devices. Simultaneously, a global connection resulting from broadband and satellite technologies has resulted in an increasing number of ‘connected users’ for information sharing. The emergence of new mobile health (mHealth) technologies has resulted from the temporal intersection of several coincidental movements: (i) an urgent need to address the rising burden of chronic diseases; (ii) Moore's law—the exponential increase in computing power resulting in the development of smaller and cheaper mobile electronics; and (iii) shifting healthcare model to an increasingly patient-centric designs. mHealth is defined by the practice of medicine supported by portable diagnostic devices. Use of these devices at the point-of-care is resulting in a change in the method of healthcare delivery from one that was health-systems generated to one that is remote and patient generated. The culmination of these factors presents unparalleled opportunities to increase patient engagement, to reduce healthcare costs, and to improve outcomes. To reach the transformative potential of mHealth, a great deal of validation of the technical capabilities and accuracy, as well as the clinical impact of these technologies, is needed before we know they are effective. The real-world practice of medicine is complex and raises important questions on how we can generate clinically meaningful digital health data. Clinicians are beginning to enquire whether more devices necessarily mean more information and if some information may be redundant or even unnecessary. As mHealth devices become increasingly available, three important questions arise: who should be the first digital health adopter: the patient, the provider, or the healthcare system? What factors of mHealth are most effective? And what is the evidence supporting the clinical utilization of such devices? As we aim to determine the effectiveness of these technologies, what are the outcomes—morbidity and mortality—or are patient-generated outcomes such as quality of life equally important? Are patients prepared to understand mHealth findings particularly elderly patients or those with complex disease states? Do patients modify their behaviour? Will user-generated data lead to patients seeking out therapies for digital data rather than true disease states? We present these questions as they relate across the digital device, the digital patient, and the digital clinic (Figure 1), and discuss the literature evaluating mHealth towards their answers. Digital devices Which components of digital devices make them usable and how do these devices help to solve clinical problems? Five classifications of mHealth technologies have been developed: smartphone health ‘apps’ (>160 000 currently available), smartphone-connected devices; wearable and wireless devices; handheld-imaging platforms, and miniaturized sensor-based technologies. Conditions such as hypertension, diabetes, and heart failure (HF), as well as medication adherence monitoring, have seen significant advances across most technological categories. As new technologies are devloped, data transfer becomes increasingly important, especially when considering how data derived from mHealth devices integrates into clinical workflows. In general, a closed data loop is necessary and involves a cycle initiated by the patient or provider, followed by Internet (cloud)-based data transfer, interpretation of these findings or automated algorithms, and the data being returned to the patient and provider for clinical decisions (Figure 2). Herein, we discuss several mHealth technologies that have been approved for use by EU and US regulatory authorities and how such technologies advance our understanding of common clinical problems. The mHealth data flow for clinical care. To maximize clinical care, a closed loop is necessary that involves patient- or practitioner-derived mHealth data, Internet-based data transfer interpreted by patients, practitioners, or with automated algorithms, and returned back to patients and providers for clinical decisions. Healthcare's digital future Within the next decade, we predict the development of new technologies across several areas in diagnostics, imaging, and therapeutics (Figure 3). Similar to clinical practice, the reality of mHealth is becoming increasingly complex. Our analysis of the current state of the field provides three main paths for translating mHealth to the real world: to identify new methods for patient engagement that results in beneficial and measurable behavioural changes, to develop the necessary tools to streamline clinical integration and data analytics, and to outline the regulatory factors that promote the most effective and robust technologies for clinical use. To achieve all three, we are collectively required to create an evidence base that assesses the impact of mHealth on healthcare quality, cost, and outcomes. In doing so, this interplay of digital devices, digital patients, and digital doctors holds exceptional promise for the future developments in medicine. by Garibli A. References 1. Topol EJ. Transforming medicine via digital innovation. Sci Transl Med 2010; 2: 16. 2. Topol EJ, Steinhubl SR,Torkamani A. Digital medical tools and sensors. JAMA 2015; 313: 353 –354. 3. Silva BM, Rodrigues JJ, de la Torre Díez I,López-Coronado M, Saleem K. Mobile-health: a review of current state in 2015. J Biomed Inform 2015; 56:265 –272.
If this page is in your subscriptions, then it will be removed. You will not see this page. If you want to unblock a user, go to the settings, the list of blocked users and click unblock