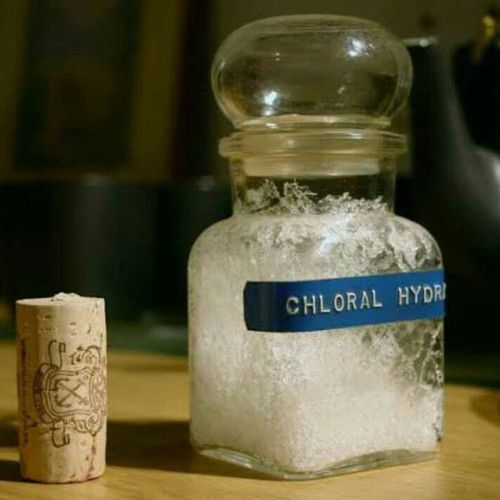
The doyen among German organic chemists during much of the nineteenth century was Justus von Liebig (1803 – 1872), the renowned Professor of Chemistry in Munich. One of his many discoveries was the volatile liquid chloroform (CHCl3), which later became important as a general anaesthetic drug. The use of chloroform as a volatile anaesthetic in surgery is credited to a Scottish physician James Young Simpson (1811 – 1870). Simpson demonstrated the benefits of chloroform to deaden the pain associated with childbirth and one of his first patients in 1872 was none other than Queen Victoria of England. In 1832, Liebig also prepared chloral hydrate and showed that in alkaline solution it was converted into chloroform and formic acid. This prompted the German physician and pharmacologist Oscar Liebreich (1839 – 1908) to investigate whether the same reaction might occur directly in the blood, which would mean that chloral hydrate might also be useful anaesthetic in the same way as chloroform. The results of these investigations were reported in a classic monograph (Figure 1.). Figure 1. Portrait of Oscar Liebreich alongside the first page of his 1869 monograph on chloral hydrate and its use as a hypnotic. Administration of chloral hydrate to animals put them into a deep sleep, but without loss of pain sensation, which meant its pharmacological effects differed from that of chloroform. Further studies showed that chloral hydrate was a relatively safe sleeping aid (hypnotic) and entered the pharmacopoeia as early as 1869 and still exists today (Noctec ) in some countries. Indeed, chloral hydrate was incriminated in the accidental death of the Playboy model Anna-Nicole Smith (1967 – 2007), who overdosed on a mixture of pharmaceuticals. Other early drugs used as a sedative-hypnotic include bromide salts, paraldehyde, and urethanes, although these were made more or less redundant when the barbiturate class of drugs appeared in the first decade of the twentieth century. Chloral hydrate was also a significant object of study in various early pharmacological experiments. In 1875, Claude Bernard tried to determine if chloral hydrate exerted its action through metabolic conversion to chloroform. This was not only the first attempt to determine whether different drugs were converted to the same metabolite in the body but also the first to measure the concentration of a particular pharmaceutical in the blood. The results were inconclusive. In 1899 and 1901 Hans Horst Meyer and Ernest Overton respectively made the major discovery that the general anaesthetic action of a drug was strongly correlated to its lipidsolubility. However, chloral hydrate was quite polar but nonetheless a potent hypnotic. Overton was unable to explain this mystery. Thus, chloral hydrate remained one of the major and persistent exceptions to this breakthrough discovery in pharmacology. This anomaly was eventually resolved in 1948 when Claude Bernard's experiment was repeated. While chloral hydrate was converted to a different metabolite than chloroform, it was found that was converted into the more lipophilic molecule 2,2,2-Trichloroethanol. This metabolite fit much better with the Meyer–Overton correlation than chloral had. Prior to this, it had not been demonstrated that general anesthetics could undergo chemical changes to exert their action in the body. Finally, chloral hydrate was also the first hypnotic to be used intravenously as a general anesthetic. In 1871, Pierre-Cyprien Oré began experiments on animals, followed by humans. While a state of general anesthesia could be achieved, the technique never caught on because its administration was more complex and less safe than the oral administration of chloral hydrate, and less safe for intravenous use than later general anesthetics were found to be. Chloral hydrate was routinely administered in gram quantities. Prolonged exposure to the vapors is unhealthy however, with a LD50 for 4-hour exposure of 440 mg/m3. Long-term use of chloral hydrate is associated with a rapid development of tolerance to its effects and possible addiction as well as adverse effects including rashes, gastric discomfort and severe kidney, heart, and liver failure. Acute overdosage is often characterized by nausea, vomiting, confusion, convulsions, slow and irregular breathing, cardiac arrhythmia, and coma. The plasma, serum or blood concentrations of chloral hydrate and/or trichloroethanol, its major active metabolite, may be measured to confirm a diagnosis of poisoning in hospitalized patients or to aid in the medicolegal investigation of fatalities. Accidental overdosage of young children undergoing simple dental or surgical procedures has occurred. Hemodialysis has been used successfully to accelerate clearance of the drug in poisoning victims. It is listed as having a "conditional risk" of causing torsades de pointes. In the United States, chloral hydrate is a schedule IV controlled substance and requires a physician's prescription. Its properties have sometimes led to its use as a date rape drug. References: 1. Alan Wayne Jones, June 2011, Drug Testing and Analysis 3(6):337-44, Early drug discovery and the rise of pharmaceutical chemistry. https://www.researchgate.net/publication/51243698_Early_drug_discovery_and_the_rise_of_pharmaceutical_chemistry 2. B. Holmstedt, G. Liljestrand, Readings in Pharmacology.Pergamon Press: London, 1963 3. W. H. Brock, Justus von Liebig: The Chemical Gatekeeper. Cambridge University Press: Cambridge, MA, 1997 4. https://en.wikipedia.org/wiki/Chloral_hydrate . By Garibli A.
If this page is in your subscriptions, then it will be removed. You will not see this page. If you want to unblock a user, go to the settings, the list of blocked users and click unblock